Blood is composed of two parts: fluid part and cellular part. The fluid part is called the plasma, in which the cells, nutrients and blood gases circulate. The cellular part composed of red blood cells (RBCs), white blood cells (WBCs) or leucocytes and platelets.
The fluid part (plasma)
The plasma constitute about 55-65% from the circulating blood. About 92% from the plasma is water. The remaining (6-8%) consists of plasma proteins (Albumin, globulins and fibrinogen), other biochemical constituents and minerals.
The cellular part or formed element:
The RBCs represent the majority of the formed elements, varied from 35-45%, the numbers of the circulating RBCs varied between human to animal species. The count in human is ranged from 4-6 x106/mm3, in horse from 6-12 x106/mm3, in cattle from 5-10.5 x106/mm3, in sheep 8-16 x106/mm3, in camel 5-8 x106/mm3, in dog 5-7.9 x106/mm3, in cat 5-10 x106/mm3. The leucocytes and platelets are counted in thousands, and represent from 1-1.5% from the circulating blood.
Erythrocytes (RBCs):
The major function of the RBCs is to transfer oxygen from the lung to tissue, through binding of oxygen (O2) to hemoglobin forming oxyhemoglobin (Oxygenated hemoglobin) and to transfer carbon dioxide (CO2) from the tissues to the lung through binding of CO2 to hemoglobin forming deoxygenated hemoglobin (Carboxy hemoglobin). Oxyhemoglobin circulate in the arteries, however, deoxyhemoglobin circulates in the venous side. The only exception is the pulmonary veins, which carry oxygenated blood from the lung to the left atrium and the pulmonary artery, which carry deoxygenated blood from the right atrium to the lung. The shape of RBCs is biconcave disc in human and most animal species, except camel and birds, where the RBCs is oval in shape. On the other hand, the RBCs are nucleated in birds and fish.
Leucocytes:
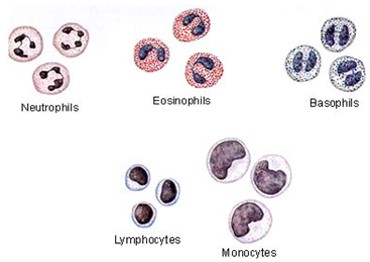
The leucocytes are classified into two major groups, which are granulocytes and agranulocytes. The granulocytes include the neutrophils, eosinophils and basophils. The agranulocytes include lymphocytes and monocytes.
The granulocytes:
The neutrophils contain fine granules (granulocytes), which stain neutral (no stain), under the light microscope. The neutrophils are called polymorphonuclear, due to the different shapes of their nucleus. The neutrophils represent the first line of defense and their major function is phagocytosis. Factors that help the neutrophils in phagocytosis are the presence of pseudopodia, which facilitate the engulfing of bacteria, and the presence of cytoplasmic granules that release chemicals to destroy phagocytized microorganisms. The Eosinophils contain large granules, which stain red (Acidophilic or eosinophilic) with Giemsa stain. The eosinophils release chemicals that destroy parasites, especially those penetrate through the skin, lung and mucous membranes, or circulate in the blood. The basophils are very rare in the blood circulation, contain basophilic granules, and their major function is to release histamine and heparin.
The agranulocytes:
Lymphocytes contain none segmented nucleus and thin layer of cytoplasm, the cytoplasm of the lymphocyte normally is clear. -Lymphocytes are classified according to the size into small, intermediate and large lymphocytes. -There are two types of lymphocytes in the blood circulation; B- lymphocyte and T lymphocytes. B cells are responsible for the humeral immunity, where they produce antibodies against invading microorganisms. T cells represent the cellular immunity, attack cells infected by viruses or cancer cells. -Monocytes are the largest leucocytic cell in the blood circulation. The plasma membrane is irregular in shape, the nucleus is large usually bean or kidney shape, and the cytoplasm is foamy or smoky and contain vacuoles. They are phagocytic cells, increased in the tissues during chronic inflammation.
Platelets:
Platelets are fragments of the megakaryocytes at the bone marrow. The most important function of platelets is the stop of bleeding. When injury to the endothelial lining blood vessels occurs, the platelets adhere to the site of injury forming the platelet plug, then secret vasoconstrictor (Serotonin) to help decrease the blood flow to the site of injury. During the process of hemostasis, the platelets secrete thromboplastin (platelets tissue factor), which initiate the process of blood coagulation by converting prothrombin to thrombin, the later activate the conversion of fibrinogen to fibrin threads, which make meshes on platelets and help to stop bleeding. The formation of excessive fibrin threads is prevented by the inhibitory effect of fibrin on thrombin. The process of stoppage of bleeding is called hemostasis. After healing of the endothelial injury, the clot stimulates the secretion of tissue plasminogen Activator (TPA), TPA stimulates the conversion of plasminogen to plasmin, the latter dissolve the clot slowly.



![Academic Opportunities at Ontario Tech University [CA]](https://scholaridea.com/wp-content/uploads/2022/07/ontario-768x432.jpg)