Liver function tests include the measurement of some chemicals that is being metabolized or synthesized by the liver. Both qualitative and quantitative evaluation is required to assess the function of the liver. The qualitative evaluation of the liver function includes physical examination of the mucous membranes (Jaundice), physical examination of feces and urine and chemical examination of urine. The quantitative evaluation include measurement the levels of chemicals in blood samples. Chemicals or metabolites usually measured to assess the liver function are hepatic enzymes, serum bilirubin, serum bile acids, serum proteins and dye excretion.
Liver function tests are used to diagnose a liver disease, assess the efficiency of treatment, differential diagnosis and prognosis.
Tests for hepatic disease are performed for a variety of purposes include confirming the existence of liver disease, assessing the nature (e.g., hepatocellular injury, cholestasis) and severity of the disease to determine prognosis, monitoring the clinical course and response to therapy, and screening individuals at risk for the existence of occult liver disease.
Conventional tests for hepatic disease provide information about the integrity of the hepatocytes (ALT, AST, SDH) and the status of the biliary system (AP, GGT). Hepatic function can be assessed by estimating the excretory capacity (bilirubin, bile acids NH3) and synthetic functions (NH 3 /urea, albumin, fibrinogen, and prothrombin) of the liver.
- Hepatic enzymes
Hepatic enzymes are not used to directly assess the function of the liver, but indicate alteration in the integrity of the hepatocytes or the epithelial cells of the biliary tract. Hepatic enzymes have a known function inside the liver epithelial cells and being released when the cells are damaged as in case of hepatic necrosis, acute or chronic inflammation.
There are two major groups of hepatic enzymes; the first group includes liver enzymes that are released after hepatic necrosis as aspartate aminotransferase (AST), alanine aminotransferase (ALT), glutamic dehydrogenase (GD), sorbitol dehydrogenase (SD) and arginase. The second group contains hepatic enzymes that are released following intrahepatic or extrahepatic cholestasis as glutamyltranspeptidase (GGT), alkaline phosphatase (ALP) and 5’nucleotidase (5′-ND).
1.a. Serum aspartate and alanine aminotransferase
AST and ALT are used inside the liver cells to transfer the α-amino nitrogen of asparatate or alanine from AST or ALT respectively to α-ketoglutaric acid, which result in the formation of glutamate or pyruvate. The latter two compounds are utilized by the liver in gluconeogenesis and for synthesis of urea. On the other hand, alanine is formed in the muscle by transamination of pyruvate, then alanine is transported to the liver.
The activity of ALT is high in the liver of human, cat, dog and rodents. Serum ALT is used for diagnosis of liver diseases in these species. However, liver ALT is low in case of herbivorus animals (Horse, cattle, ovine, caprine).
The activity of AST is high in the liver of all domestic animals, but it is not specific for the liver, this because AST activity is high also in the skeletal muscles, heart and kidney. AST cannot be used alone for diagnosis of a hepatic disease.
Serum AST and ALT activities increased after hepatocellular injury or necrosis and also in case of acute and chronic inflammation. Their levels can be used to evaluate the response to therapy, as their activities decrease in serum in response to recovery. Measuring serum AST activity alone cannot be used for diagnosis of hepatic disease. The source of serum AST can be traced if the source is skeletal muscles, this can be done through measuring creatine phosphokinase (CK), which is released from the skeletal muscles in response to trauma or disease. CK is specific for skeletal muscle injury and released before AST, the elevation of both AST and CK activities indicate the source of AST is the skeletal muscles and not the liver. ALT is also released from the muscles in severe muscle disease.
1.b. Sorbitol dehydrogenase (SDH)
Sorbitol dehydrogenase is a zinc metalloenzyme, responsible for the conversion of sorbitol to fructose. SDH activity is high in the liver and kidney, and used in the evaluation of hepatocellular injury in most animal species including dog, horses and ruminants. SDH is disappear rapidely from serum and its activity must be measured within 8-12 hours from sampling.
1.c. Glutamate dehydrogenase (GD)
Glutamate dehydrogenase is a mitochondrial enzyme and plays a key role in detoxification of ammonia. GD scavenges the ammonia by elimination of α-ketoglutarate to form glutamate. Serum GD is elevated in case of hepatic necrosis in ruminants.
- d. Alkaline phosphatase (ALP)
Alkaline phosphatases are group of zinc metalloenzymes, which present in high concentrations in liver, bone, kidney and intestine. The actual physiological function of ALP is not fully understood, but it may play a role in transport function of the cells or may play a role in bone calcifications.
ALP is principally released from the liver and bones. Serum ALP is elevated in cases of diseases affecting the bile duct including cholangitis, biliary cirrhosis and obstruction. Unlike serum AST and ALT, the release of serum ALP is not released from damaged liver cells. High serum ALP level is related to increase the intrahepatic synthesis and the newly synthesized enzyme is released to the circulation. High serum ALP level was observed in cholestasis, partial hepatectomy and in infiltrative diseases of the liver (Intrahepatic cholestasis). Partial hepatectomy stimulates increased synthesis of ALP in the regenerated tissues.
- e. γ –Glutamyltranspeptidase (GGT)
γ –Glutamyltranspeptidase is a membrane bound enzyme that catalyzes the transfer of γ –glutamyl group from γ –glutamylpeptides such as glutathione to other amino acids or peptides. GGT is present in high concentration in the liver and kidney. Serum GGT is elevated in diseases affecting the hepatobiliary system associated with cholestasis. High urinary GGT activity is used for diagnosis of kidney diseases.
High serum GGT and ALP activities are good indicators for diseases affecting the biliary system and cholestasis. Higher serum GGT with normal ALP is characteristic for diseases affecting the hepatocytes.
2. Serum Bilirubin
2.a. Bilirubin
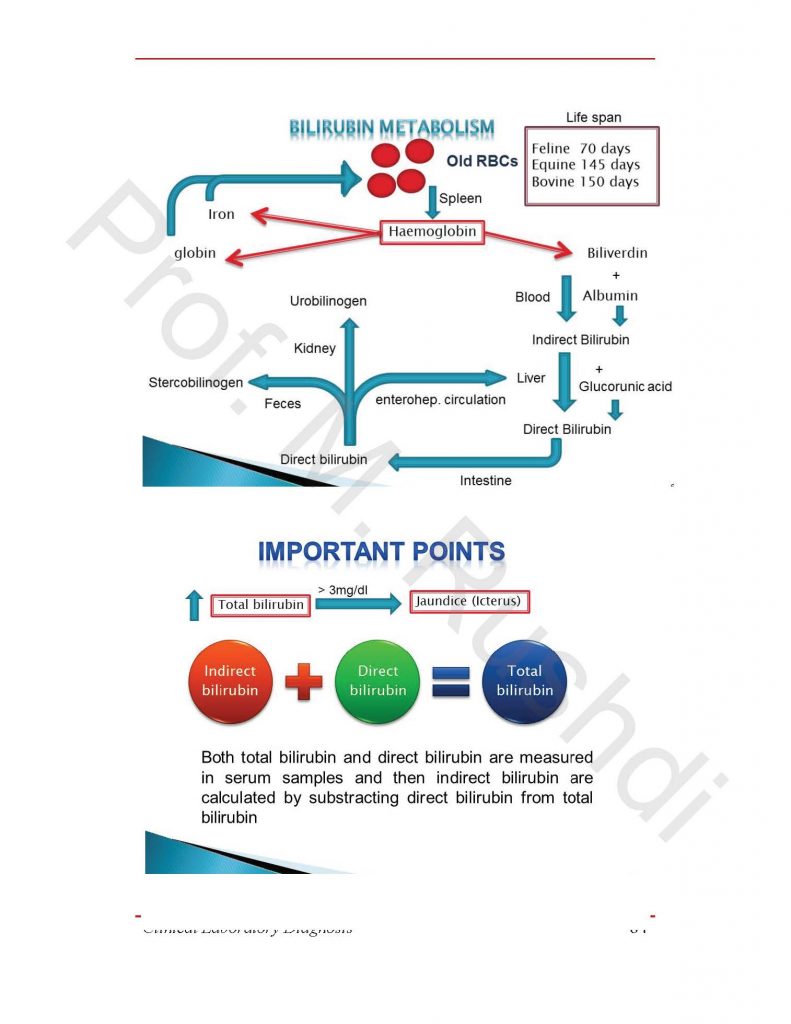
- Bilirubin is a by-product of hem breakdown. In its initial form it is not water-soluble and when in the plasma it is bound to albumin. It is transported via the reticulo-endothelial system to the liver where it is rendered soluble by conjugation with glucuronic acid and other substances. The bilirubin conjugate is excreted in the bile, and it and its associated pigments (mainly stercobilin) are responsible for the characteristic brown colour of faeces. On laboratory request forms ‘total bilirubin’ means just that. ‘Direct bilirubin’ is conjugated bilirubin, and the unconjugated (or indirect) bilirubin is calculated by subtraction from the total.
- Oral administration of broad-spectrum antibiotics may diminish the metabolic activity of intestinal bacteria and result in a negative test for urobilinogen in the urine in the absence of cholestasis.
2.b. Jaundice
Jaundice or icterus is defined as the yellowish pigmentation of skin and mucous membranes especially conjunctiva and sclera, as a consequence of increased blood bilirubin level.
There are two forms of bilirubin in the blood circulation, which are direct or conjugated and indirect or unconjugated bilirubin. The increase of any one of them result in increased the total bilirubin level, which cause the yellowish color of skin.
Normally total bilirubin level in adult animals is below 1 mg/dl,
Jaundice occurs when the total bilirubin level become above 3 mg/dl.
Under normal physiological conditions, bilirubin is formed from the normal breakdown of aged erythrocytes by the reticuloendothelial cells, which leads to the formation of biliverdin. The latter is transferred in the blood binding to albumin. The combination of albumin and biliverdin is called indirect bilirubin. Increase breakdown of RBCS as in hemolytic anemia results in increased blood biliverdin level and subsequently high blood indirect bilirubin level.
Indirect bilirubin is removed from the blood by the liver, where indirect bilirubin is conjugated with glucuronic acid, hence it name is changed from indirect bilirubin to direct bilirubin (Conjugated). Direct bilirubin pass from the hepatocytes to the bile canaliculi, and then to the main bile duct and finally to the small intestine.
In the small intestine, direct bilirubin is converted to stercobilinogen by the action of bacteria. There are three pass ways for the stercobilinogen; the first is by excreting it in the feces, which give the brown color of feces. The second is by absorption through the portal circulation (Enterohepatic circulation, where direct bilirubin is returned to the blood. The third pass way is through the excretion of stercobilinogen in urine, and its name changed to urobilinogen.
Direct bilirubin is increased in the blood in case of obstruction of the main bile duct, intrahepatic cholestasis and in case of hepatitis.
2.c. Types of jaundice
There are three types of Jaundice; pre-hepatic (Hemolytic), hepatic jaundice and post-hepatic (Obstructive) Jaundice.
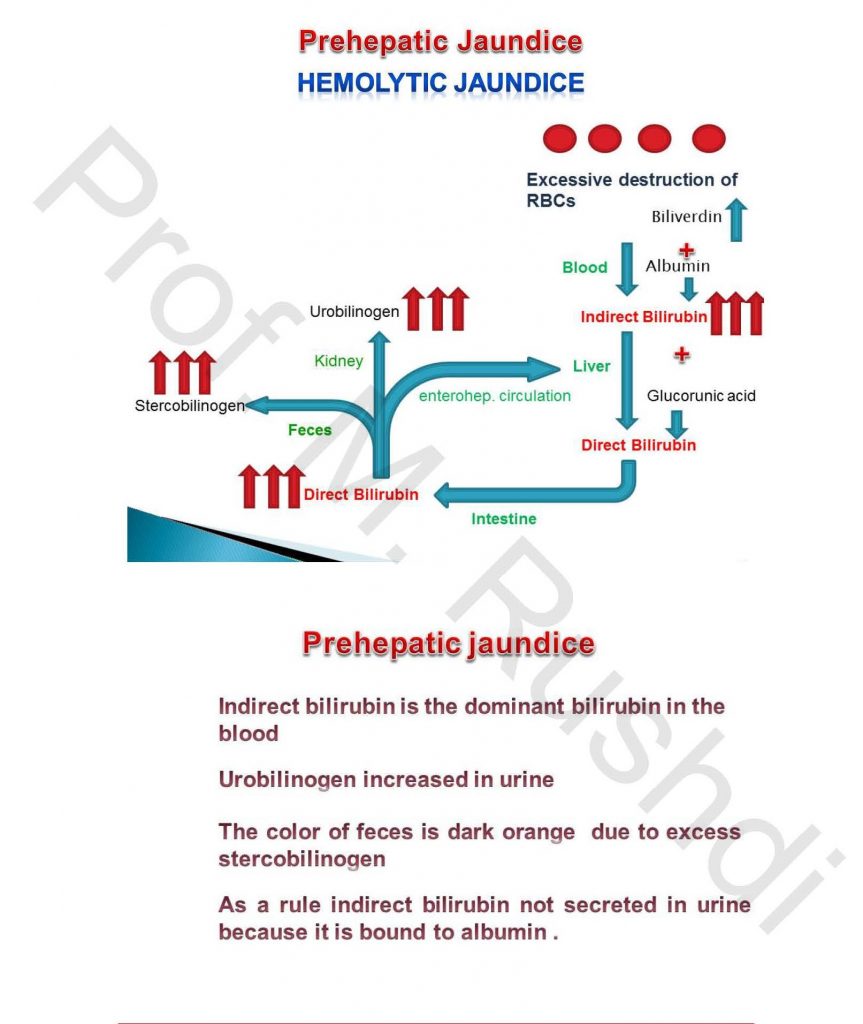
Prehepatic (Hemolytic) jaundice
- Occurs in case of hemolytic anemia.
- Total bilirubin level is increased due to increased blood indirect bilirubin level.
- The color of urine remains normal, because indirect bilirubin is bind to albumin, and subsequently unable to pass the glomerular filter.
- Higher level of blood indirect bilirubin, results in higher bilirubin uptake by the liver and increased the rate of formation of direct bilirubin, and increased the direct bilirubin that pass to the small intestine. This results in dark brown color of the feces.
- The increased stercobilinogen level in the small intestine results in increase the formation of urobilinogen, which is excreted in urine.
- The most important changes in pre-hepatic jaundice are increased total and indirect bilirubin in blood, normal urine color, dark brown feces and increased urobilinogen in urine.
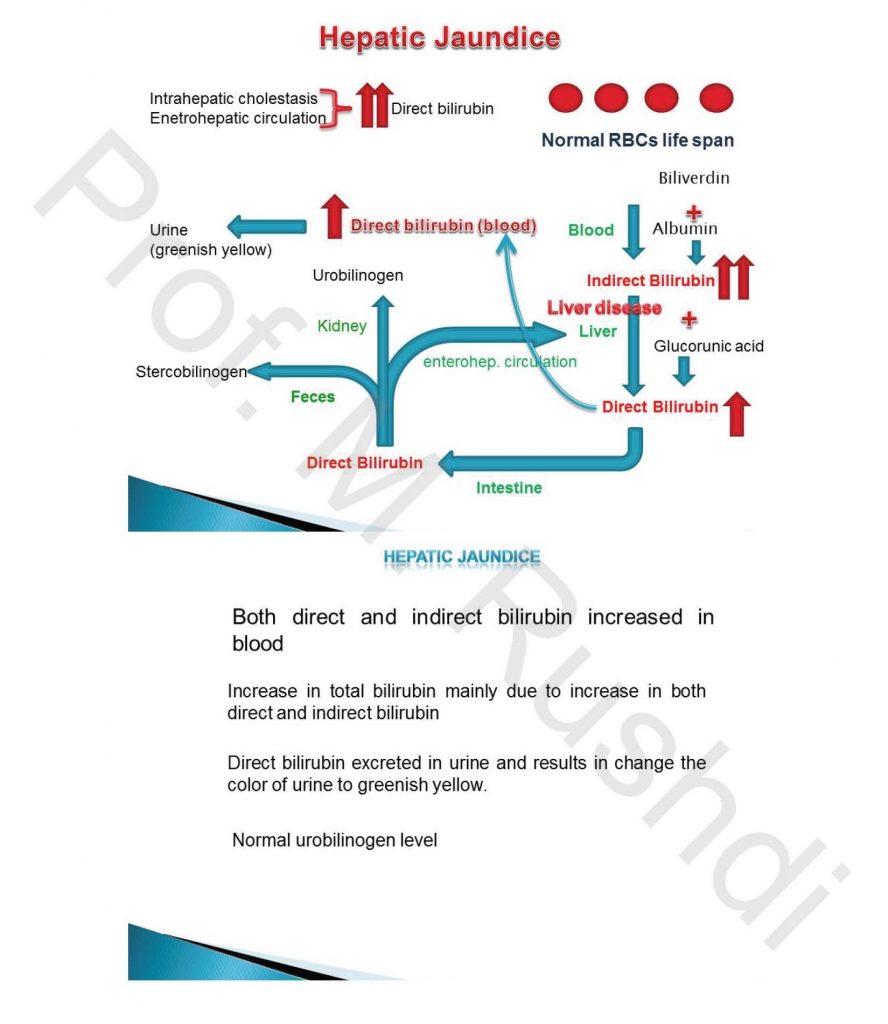
Hepatic jaundice
- Occurs in case of hepatitis.
- Total bilirubin level increased due to increase of both direct and indirect bilirubin.
- Dark brown color of urine, as a result of excretion of direct bilirubin in urine.
- Normal color of feces
- Normal urobilinogen level
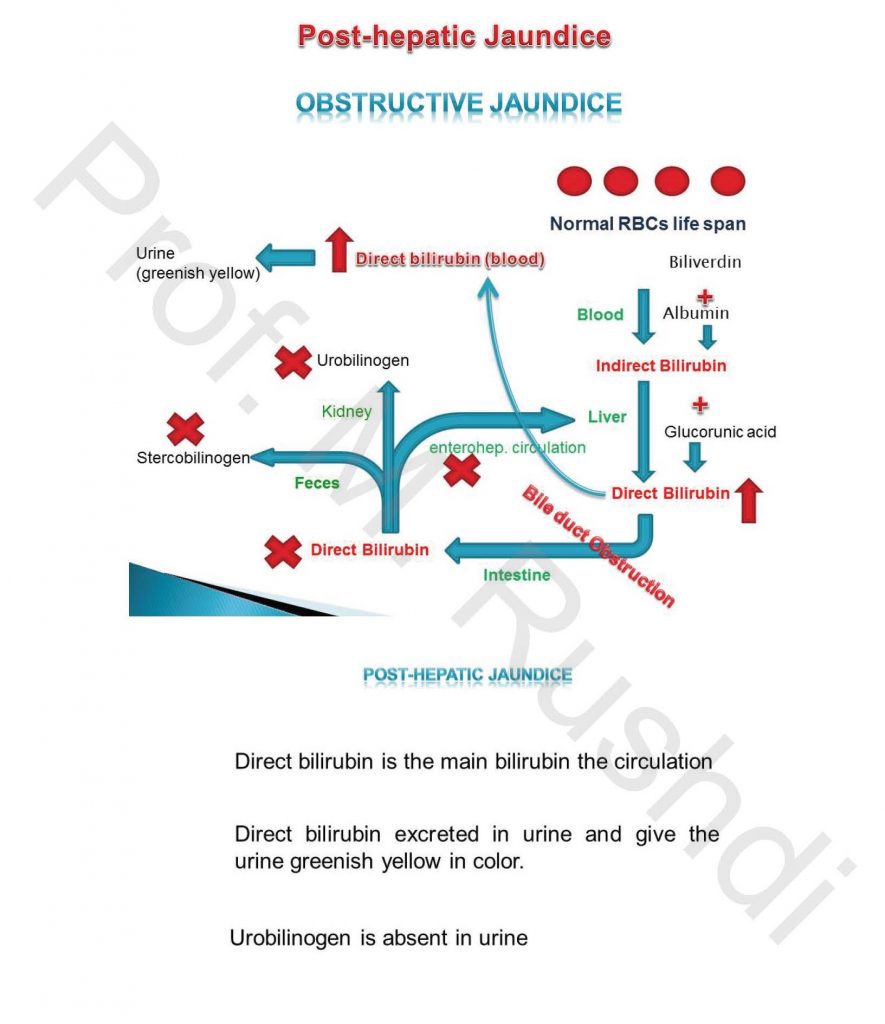
Post-hepatic (Obstructive) Jaundice
- Occurs in case of obstruction of main bile duct.
- Total bilirubin increased due to increase blood direct bilirubin level.
- Dark brown color of urine.
- Clay color of feces
- Absence of urobilinogn from urine.
3. Serum bile acids
There are two types of bile acids; primary and secondary bile acids. Primary bile acids are synthesized from cholesterol in the liver. Primary bile acids for the most species include cholic acid and chenodeoxycholic acid.
Following synthesis, primary bile acids are conjugated either with taurine or glycine and transported across the bile canalicular membrane. Bile acids are transported from the canaliculus through bile ducts to the lumen of the duodenum. In the duodenum and jejunum, bile acids have an important role in the digestion and absorption of dietary fat and other lipids including fatsoluble vitamins.
In the terminal ileum, almost all of the bile acids secreted by the liver are absorbed by highly efficient transport mechanisms of the ileal epithelium and enter the hepatic portal vein. Normally, only a small fraction (5%) of the bile acids that enter the duodenum reach the large intestine where bacteria are responsible for deconjugation and for the formation of secondary bile acids by dehydroxylation. Dehydroxylation of cholic acid at the 7 α position results in formation of deoxycholic acid, and 7 α dehydroxylation of chenodeoxycholic acid results in production of lithocholic acid. The secondary bile acids formed in the large intestine may be absorbed and return to the liver by the enterohepatic circulation or excreted in the feces.
Serum bile acid concentrations increase with hepatocellular damage, cholestasis, or shunts from the portal system to the vena cava. Increases are highest with biliary obstruction and portosystemic shunts.
4. Plasma proteins
There are a variety of plasma proteins synthesized by the liver including albumin, α and β globulins, coagulation factors (fibrinogen (I), prothrombin (II), V, VII, IX, X, XI), plasma proteins of the complement system, plasmin, α -1-antitrypsin and α -2-macroglobulin.
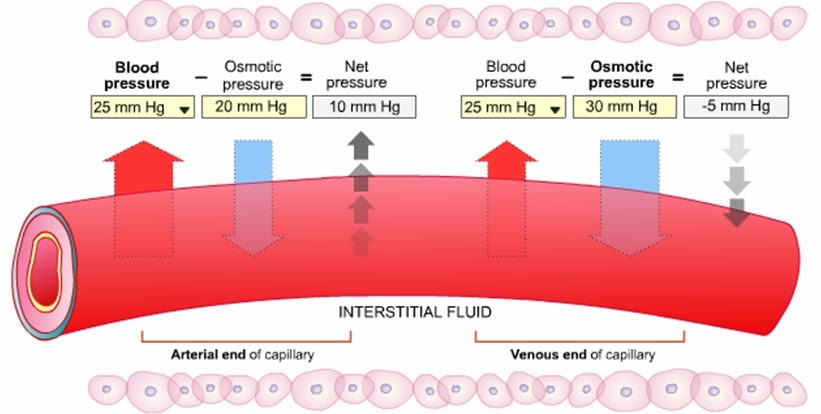
Albumin is the major plasma proteins in the blood, synthesized mainly by the liver. Albumin has two important functions. It is the most important for keeping the oncotic or osmotic pressure of the circulating blood constant, which help to prevent the loss of fluid in the interstitial tissues. One of the functions of albumin is to maintain intravascular oncotic (colloid osmotic) pressure. To facilitate movement of fluid throughout the body, the average capillary pressure is 15 to 25 mm Hg greater at the arterial end than at the venous end. Starling’s law describes forces that determine fluid movement across the capillary membrane. Balance between pressures on each side of the capillary membrane is related to hydrostatic pressure pushing fluid out of some capillaries and osmotic pressure pulling fluid back into other capillaries. There is also a small amount of fluid that does not follow this path but leaks through and is returned by way of the lymphatics.
In addition to maintaining colloid oncotic pressure, albumin also facilitates transportation of substances. These substances include bilirubin, metals, ions, enzymes, amino acids, hormones, free fatty acids, drugs, and phospholipids. Albumin is essential for the metabolism and detoxification of many of these substances.
Hypoalbuminemia is associating diseases that decrease the albumin synthesis (chronic liver diseases) or increase the albumin loss through the gastrointestinal (severe intestinal inflammation) or urinary tract (glomerulopathy). The decrease blood albumin level results in the inability of the body to withdraw the fluids from the interstitial tissues. The accumulation of fluids results in edema, ascitis and pulmonary edema.
Fibrinogen is a glycoprotein synthesized in the liver, and it is one of the coagulation factors that play an important role in the formation of clot as fibrinogen is converted to fibrin threads by thrombin at the site of blood vessel injury, which result in the formation of blood clots. Also, fibrinogen is an acute phase protein, its plasma level is elevated in cases of inflammation. Plasma fibrinogen is decreased in case of chronic liver diseases. The deficiency of fibrinogen leads to bleeding tendency and characterized by increased bleeding and coagulation times.
Prothrombin is an essential blood coagulation factor that is synthesized in the liver, where vitamin K is converted into prothrombin in the hepatocytes. Consequently, any disease or condition that affects the absorption or the process of conversion inside the hepatocytes will results in hypoprothrombinemia. Vitamin K absorption from the small intestine is decreased in cases of primary deficiency in the diet and absence of bile pigment (essential for absorption of fat). Warfarin poisoning (inhibit the conversion of vitamin K into prothrombin). Liver cirrhosis affects the synthesis of prothrombin from vitamin K. Hypoprothrombinemia results in prolonged prothrombin time, and coagulation times.
Plasmin is synthesized by the liver and it is essential for degradation of fibrin.
The liver also is the site of synthesis of the protease inhibitor α -1-antitrypsin. It is generally known as serum trypsin inhibitor. It protects tissues from enzymes of inflammatory cells, especially neutrophil elastase, Neutrophils mobilize, delivering elastase at the alveolar surface in response to bacterial infections, environmental pollutants, or tobacco exposure. α -1-antitrypsin has a reference range in blood of 1.5 – 3.5 gram/liter (in US the reference range is generally expressed as mg/dL or micromoles), but the concentration can rise many fold upon acute inflammation. In its absence, neutrophil elastase is free to break down elastin, which contributes to the elasticity of the lungs, resulting in respiratory complications such as emphysema, or COPD (chronic obstructive pulmonary disease) and cirrhosis.
The liver also is the site of synthesis of α -2-macroglobulin, an inhibitor of a variety of other proteases. It functions as an inhibitor of fibrinolysis by inhibiting plasmin. It functions as an inhibitor of coagulation by inhibiting thrombin. Alpha-2-macroglobulin may act as a carrier protein because it also binds to numerous growth factors and cytokines, such as platelet-derived growth factor, basic fibroblast growth factor and insulin.
The complement system consists of a number of small proteins found in the blood, in general synthesized by the liver. The complement system is an enzyme cascade that is a collection of blood and cell surface proteins to help the abilities of antibodies to clear pathogens from an organism. The complement system that comprises 30 different proteins, including serum proteins, serosal proteins, and cell membrane receptors is an important part of the innate immune system. The complement system has four major function, including lysis of infectious organisms, activation of inflammation, opsonization and immune clearance.
5. Dye excretion
Dye clearance test is used to measure the hepatic function in cases were occult liver disease exist, without prominent clinical signs. Dye clearance test should not used in patients with prominent signs of hepatic disease. Dyes mostly used are bromosulphophthaline (BSP) and isocyanine green (ICG). The principle of the test is depend on the fact that BSP and ICG are not toxic and are excreted only through the liver. The dye is injected intravenously in a dose calculated based on the body weight, and then the rate of clearance is calculated by spectrohpotometeric measurement of its blood concentration at different intervals.
The dose of BSP dye is 5mg/kg in dogs and cats, in adult horse (450kg) the dose is 1 g, however in young hourse the dose is 0.5 g injected intravenously, blood sample for measurement BSP concentration is collected after 30 min.
The more serious manifestations of liver disease are hyperglycemia and hypoglycemia. In fact, patients with severe liver disease often have glucose tolerance curves very much like those seen in diabetes mellitus. That is to say, with food ingestion, they tend to become hyperglycemic because the hepatocytes cannot store glycogen while, as dietary intake is decreased or absent, the hepatocytes are not well able to mobilize glucose from what little stored glycogen there is, and so these patients have episodes of hypoglycemia. This phenomenon is sometimes called “hepatic diabetes.”
Prof. Mahmoud Rushdi
